The carotid pulse (CP) is a pressure signal acquired over the carotid artery as it passes near the surface of the body at the neck. It delivers a pulse signal signifying the variations in arterial blood pressure and volume with each heartbeat. Better to start at the radial and switch to the carotid in the 1 or 2 out of 1000 cases where the conscious adult with no obvious arm circulation issues lacked a radial pulse. The carotid pulse (CP) is a pressure signal acquired over the carotid artery as it passes near the surface of the body at the neck. It delivers a pulse signal signifying the variations in arterial blood pressure and volume with each heartbeat.
Carotid Pulse +2
- The carotid artery can be positioned close to the surface in some individuals. If a person doesnt have extensive fat tissue, and if the neck is held in certain positions its very easy to see the pulsations. Its just a variation of normal in almost all cases, with the rare rare exception of an aneurysm.
- Carotid Artery: Plateau pulse – slow rise and slow collapse pulse; may be caused by aortic stenosis, slow ejection of blood through a narrowed aortic valve. Decreases amplitude (grade point pulse) – due to hemorrhagic shock, pulse is weak due to decreased blood volume.
Also found in: Dictionary, Thesaurus, Encyclopedia.
pulse
[puls] 2. the beat of the heart as felt through the walls of a peripheral artery, such as that felt in the radial artery at the wrist. Other sites for pulse measurement include the side of the neck (carotid artery), the antecubital fossa (brachial artery), the temple (temporal artery), the anterior side of the hip bone (femoral artery), the back of the knee (popliteal artery), and the instep (dorsalis pedis artery).What is felt is not the blood pulsing through the arteries (as is commonly supposed) but a shock wave that travels along the walls of the arteries as the heart contracts. This shock wave is generated by the pounding of the blood as it is ejected from the heart under pressure. It is analogous to the hammering sound heard in steam pipes as the steam is forced into the pipes under pressure. A pulse in the veins is too weak to be felt, although sometimes it is measured by sphygmograph (see below); the tracing obtained is called a phlebogram.
The pulse is usually felt just inside the wrist below the thumb by placing two or three fingers lightly upon the radial artery. The examiner's thumb is never used to take a pulse because its own pulse is likely to be confused with that of the patient. Pressure should be light; if the artery is pressed too hard, the pulse will disappear entirely. The number of beats felt in exactly 1 minute is the pulse rate.
In taking a pulse, the rate, rhythm, and strength or amplitude of the pulse are noted. The average rate in an adult is between 60 and 100 beats per minute. The rhythm is checked for possible irregularities, which may be an indication of the general condition of the heart and the circulatory system.
The amplitude of a pulse can range from totally impalpable to bounding and full; however, such terms are vague and subject to misinterpretation. To provide a more standardized description of pulse amplitude some agencies and hospitals use a scale that provides a more objective evaluation and reporting of the force of a pulse. On such a scale zero would mean that the pulse cannot be felt; +1 would indicate a thready, weak pulse that is difficult to palpate, fades in and out, and is easily obliterated with slight pressure; +2 would be a pulse that requires light palpation but once located would be stronger than a +1; +3 would be considered normal; and a +4 pulse would be one that is strong, bounding, easily palpated, and perhaps hyperactive, and could indicate a pathological condition such as aortic regurgitation.
If a pulse is noted to be weaker during inhalation and stronger during exhalation (pulsus paradoxus), this could indicate either greater reduction in the flow of blood to the left ventricle than is normal, as in constrictive pericarditis or pericardial effusion, or a grossly exaggerated inspiratory maneuver, as in tracheal obstruction, asthma, or emphysema.
An instrument for registering the movements, form, and force of the arterial pulse is called a sphygmograph. The sphygmographic tracing (or pulse tracing) consists of a curve having a sudden rise (primary elevation) followed by a sudden fall, after which there is a gradual descent marked by a number of secondary elevations.
ca·rot·id pulse
ca·rot·id pulse
(kă-rot'id pŭls)ca·rot·id pulse
(kă-rot'id pŭls)Want to thank TFD for its existence? Tell a friend about us, add a link to this page, or visit the webmaster's page for free fun content.
Link to this page:
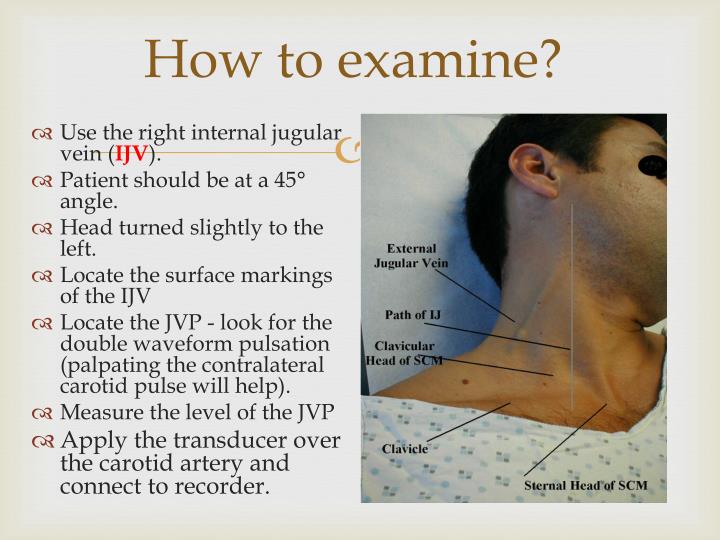
After you measure the JVP, move on to assessment of the carotid pulse. The carotid pulse provides valuable information about cardiac function and is especially useful for detecting stenosis or insufficiency of the aortic valve. Take the time to assess the quality of the carotid upstroke, its amplitude and contour, and presence or absence of any overlying thrills or bruits.
For irregular rhythms, see Table 3-10, Selected Heart Rates and Rhythms (p._), and Table 3-4,
Selected Irregular Rhythms (p._).
To assess amplitude and contour, the patient should be lying down with the head of the bed still elevated to about 30°. When feeling for the carotid artery, first inspect the neck for carotid pulsations. These may be visible just medial to the sternomastoid muscles. Then place your left index and middle fingers (or left thumb11) on the right carotid artery in the lower third of the neck, press posteriorly, and feel for pulsations.
A tortuous and kinked carotid artery may produce a unilateral pulsatile bulge.
J^ll Although there is a widespread prejudice against using thumbs to assess pulses, they are useful for palpating large arteries.
Decreased pulsations may be caused by decreased stroke volume, but may also be due to local factors in the artery such as atherosclerotic narrowing or occlusion.
J^ll Although there is a widespread prejudice against using thumbs to assess pulses, they are useful for palpating large arteries.
Press just inside the medial border of a well-relaxed sternomastoid muscle, roughly at the level of the cricoid cartilage. Avoid pressing on the carotid sinus, which lies at the level of the top of the thyroid cartilage. For the left carotid artery, use your right fingers or thumb. Never press both carotids at the same time. This may decrease blood flow to the brain and induce syncope.
Slowly increase pressure until you feel a maximal pulsation, then slowly decrease pressure until you best sense the arterial pressure and contour. Try to assess:
Pressure on the carotid sinus may cause a reflex drop in pulse rate or blood pressure.
See Table 3-9, Abnormalities of the Arterial Pulse and Pressure Waves (p. __).
■ The amplitude of the pulse. This correlates reasonably well with the pulse pressure.
■ The contour of the pulse wave, namely the speed of the upstroke, the duration of its summit, and the speed of the downstroke. The normal upstroke is brisk. It is smooth, rapid, and follows S1 almost immediately. The summit is smooth, rounded, and roughly midsystolic. The downstroke is less abrupt than the upstroke.
■ Any variations in amplitude, either from beat to beat or with respiration.
Thrills and Bruits. During palpation of the carotid artery, you may detect humming vibrations, or thrills, that feel like the throat of a purring cat. Routinely, but especially in the presence of a thrill, you should listen over both carotid arteries with the diaphragm of your stethoscope for a bruit, a murmur-like sound of vascular rather than cardiac origin.
You should also listen for bruits over the carotid arteries if the patient is middle-aged or elderly or if you suspect cerebrovascular disease. Ask the patient to hold breathing for a moment so that breath sounds do not obscure the vascular sound. Heart sounds alone do not constitute a bruit.
Further examination of arterial pulses is described in Chapter 14, The Peripheral Vascular System.
The Brachial Artery. The carotid arteries reflect aortic pulsations more accurately, but in patients with carotid obstruction, kinking, or thrills, they are unsuitable. If so, assess the pulse in the brachial artery, applying e techniques described above for etermining amplitude and contour.
se the index and middle fingers or humb of your opposite hand. Cup
Normal Carotid Pulse Rate
Small, thready, or weak pulse in cardiogenic shock; bounding pulse in aortic insufficiency (see p._).
Delayed carotid upstroke in aortic stenosis
Pulsus alternans, bigeminal pulse (beat-to-beat variation); paradoxical pulse (respiratory variation)
A carotid bruit with or without a thrill in a middle-aged or older person suggests but does not prove arterial narrowing. An aortic murmur may radiate to the carotid artery and sound like a bruit.
your hand under the patient's elbow and feel for the pulse just medial to the biceps tendon. The patient's arm should rest with the elbow extended, palm up. With your free hand, you may need to flex the elbow to a varying degree to get optimal muscular relaxation.
Continue reading here: The Heart
Was this article helpful?




